Colour vision is important in our daily life in order to let us perceive better images about our living environment. Colour vision is the ability to discriminate between different colours. Our colour vision perception is also known as photopic vision, which is appreciated by cones cells. The cones cell is mainly located at the centre part of the retina, which is the fovea area. There are 3 primary colours sensed by the cones cell in fovea which are blue, red and green. Sensation of other colours such as white, yellow, orange, purple can be produced by mixing the 3 primary colours in different combinations.

3 Primary colours
Various tests that can be used to diagnose colour vision deficiency in our clinical field. The Ishihara chart is the most common and simple test that we always use to diagnose colour vision deficiency, especially red-green colour vision deficiency. Moreover, the Farnsworth D-15 hue test can also be used to diagnose colour vision deficiency. The Farnsworth Munsell 100 hue test was a more advanced test that we can know in more detail what exactly colour vision deficiency that the patient had. These are the common tools that we used to diagnose colour vision deficiency in the clinic.
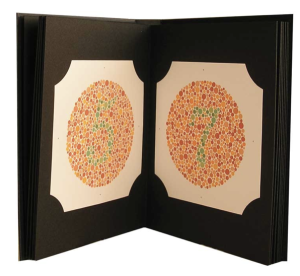
Ishihara plate

Farnsworth D-15 hue test

Farnsworth 100 hue test
Basically, colour vision deficiency can be divided into 3 categories which are deutan, protan and tritan. Deutan patients mainly will have weakness in perceiving green colour or completely cannot perceive green colour, whereas protan is the patient having difficulty in perceiving red colour or completely cannot perceive red colour. Moreover, tritan mainly will cause patient difficulty in perceiving blue colour. Colour vision deficiency can be categorised as inherited or acquired. Acquired colour vision deficiency is usually caused by drug use or some ocular disease.
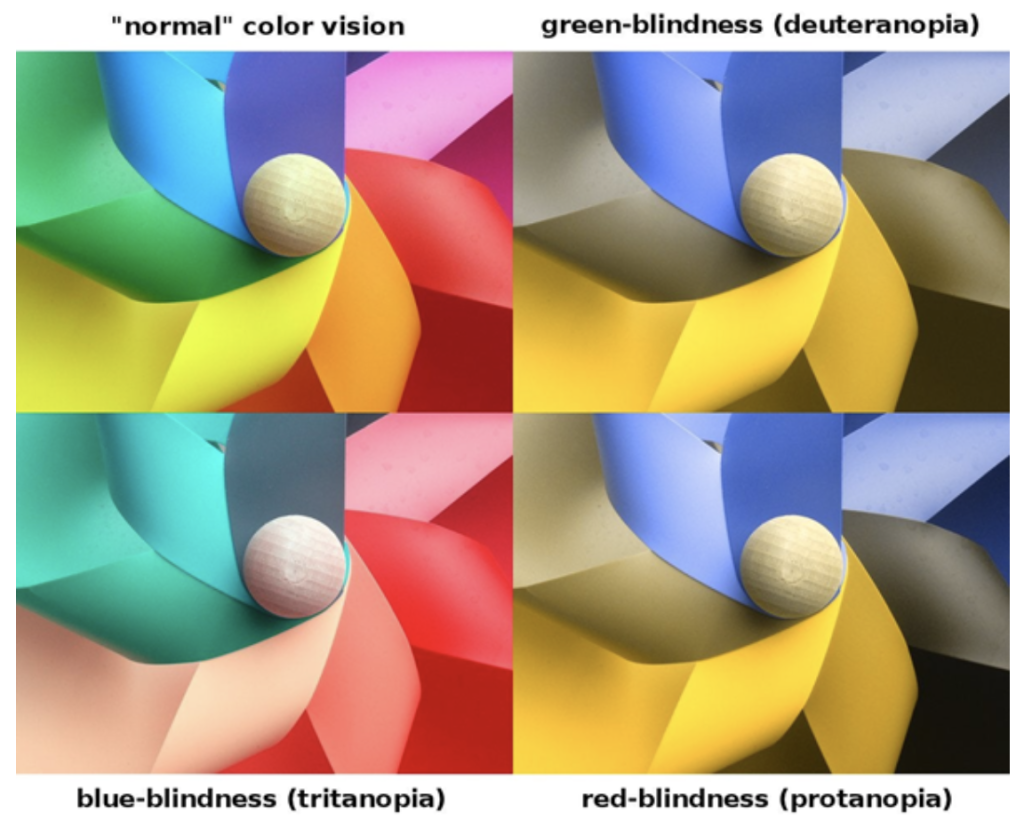
For your info, red-green colour vision deficiency is more common as compared to blue-yellow vision colour deficiency. However, male had higher risk compared to females to have colour vision deficiency as it is an X-linked disease. As male only have 1 X chromosome so if their mother passed the gene which is lack of colour vision, the son is likely to have colour vision deficiency. Females who have a father with colour vision deficiency has a 50% chance to transmit the disorder to their sons. The prevalence of colour vision deficiency worldwide is reported to be 8% in male and 0.5% in females. With early detection proper counselling can be done to the patient in order to adapt and have an idea on what is the suitable future pathway or profession that can be pursued. Hence, it is important for us to screen for colour vision deficiency especially in young male children as they have higher prevalence in getting inherited colour vision deficiency.
There are no available treatments for colour deficiency at the moment. However, there are special tinted lenses or contact lenses that can help the patient to have better perception of the colour. Early detection of colour vision deficiency since young children is vital in order to overcome the limitations such as future career pathways. We don’t treat colour vision deficiency people as disabled as they only have difficulty in differentiating colour, but the vision was usually normal. We can always provide guidance and advice for colour vision deficiency patients in choosing the right pathway or profession in the future. For acquired colour vision deficiency, we can treat the underlying problem in order to resolve the colour vision deficiency problem. Therefore, it encourages parents to bring their children to visit an eye specialist/ophthalmologist for a proper consultation which includes colour vision screening, especially for male children.



 Symptoms of Hyperopia/Far-sightedness
Symptoms of Hyperopia/Far-sightedness



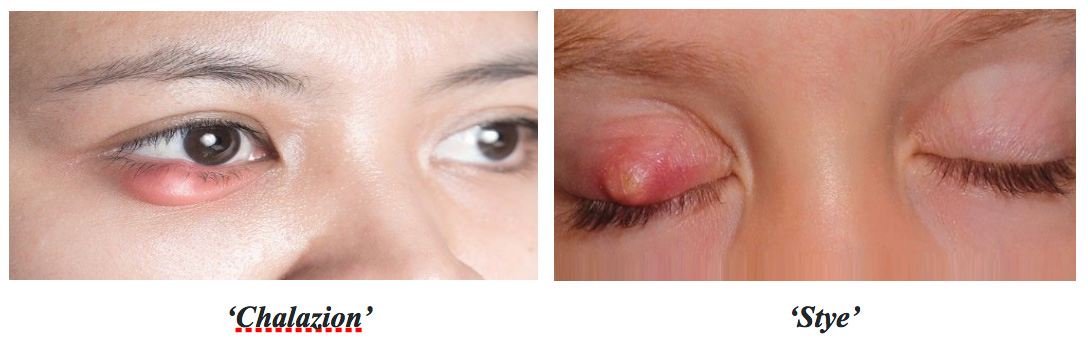 Bagaimanakah cara untuk anda menyembuhkan ketumbit?
Bagaimanakah cara untuk anda menyembuhkan ketumbit?