Ptosis (toh-SIS) is short for blepharoptosis. Ptosis is known as the dropping or falling of the upper eyelid over the eye. This happens when the border of the upper eyelids fall into a lower position than normal. In mild cases the upper eyelid might just droop a little, which is barely noticeable. However, in more severe cases it can cover the pupil which blocks the light from entering the eye and this can affect vision. Ptosis can present in one eye or both eyes. It can happen in both children and adults. The great news is this eye condition can be treated to improve vision as well as appearance cosmetically which helps improve the quality of life.
The three main reasons for droopy eyelids are dropping of the eyebrow, excessive skin of the upper eyelid and the dropping of the actual upper eyelid by itself. Ptosis can be congenital or acquired. Congenital ptosis normally presents at birth and occurs when the muscle that lifts the eyelid known as levator muscle does not develop well. Common signs of ptosis seen in children is a drooping eyelid or the upper eyelid creases are not aligned evenly with each other. Usually a child with ptosis will try to move their head back, lift up their chin, or raise their eyebrows in order to see well. Gradually, these will cause a child to have head and neck problems. In more severe cases, droopy lids that cover the pupil will affect the vision as well. In the long term, it can cause amblyopia or lazy eye. Some children with ptosis can develop astigmatism, strabismus or crossed eyes.

Acquired ptosis usually happens in later life in adults due to aging where the levator muscle stretches or separates away from the eyelid. This can happen by an eye injury (trauma) as well. Sometimes, acquired ptosis can also present after an eye surgery such cataract, botox injection, contact lens wear, tumours, in neurological disorder or systemic disease. Therefore, droopy eyelids can be a warning sign of severe medical problems.
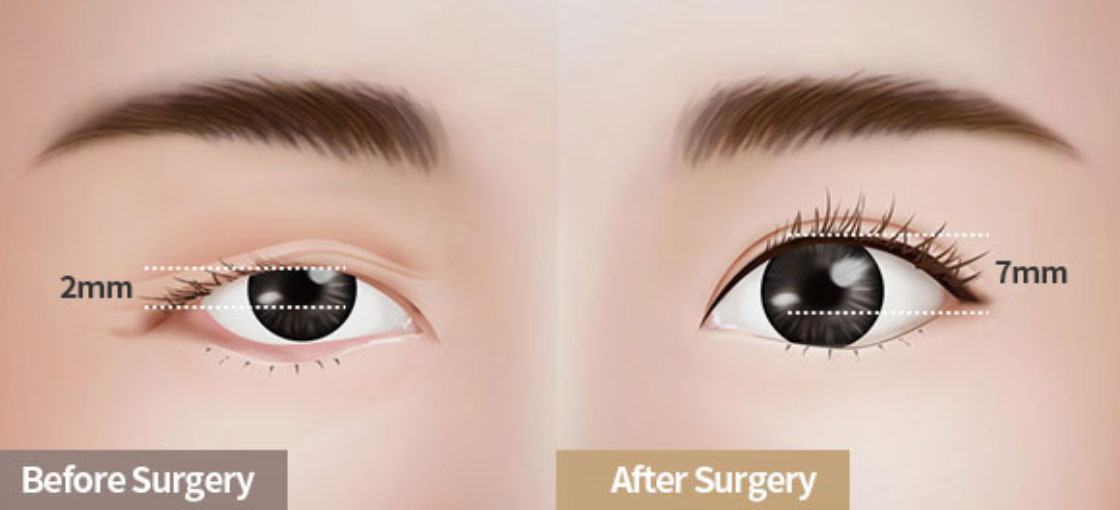
A series of eye examinations will be done by an ophthalmologist to rule out the cause of droopy eyelids for better treatment outcome. Common eye examinations include vision test and refraction especially in children to improve their vision. In moderate and severe droopy eyelids cases, surgical treatment is required for proper vision development to avoid amblyopia (lazy eyes) and poor vision. Surgical treatment for patients with normal levator muscle function is done by tightening the levator muscles that lift up eyelids and hence improve vision and appearance. In advanced cases, for patients with poor levator muscle function, the surgery is done by attaching the eyelid under the eyebrow with a sling which will help to lift the upper lid and improve vision.
Residents within Klang Valley in areas such as Cheras, Puchong, Shah Alam, Petaling Jaya, and Kepong can come visit our oculoplastic surgeon, Dr Tai Lai Yong to have their eyes examined.

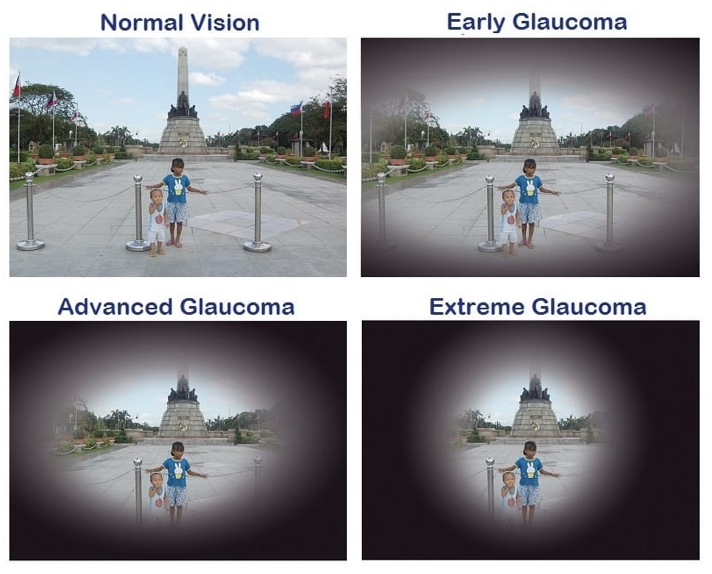 What makes glaucoma more dangerous is that the most common type of glaucoma does not show any obvious symptoms, hence goes undetected in many people. Thus, glaucoma is known as the “
What makes glaucoma more dangerous is that the most common type of glaucoma does not show any obvious symptoms, hence goes undetected in many people. Thus, glaucoma is known as the “