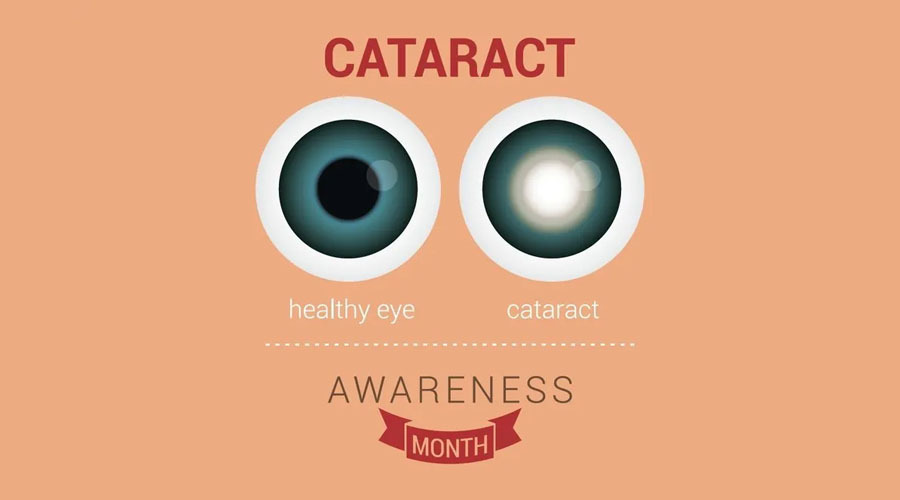
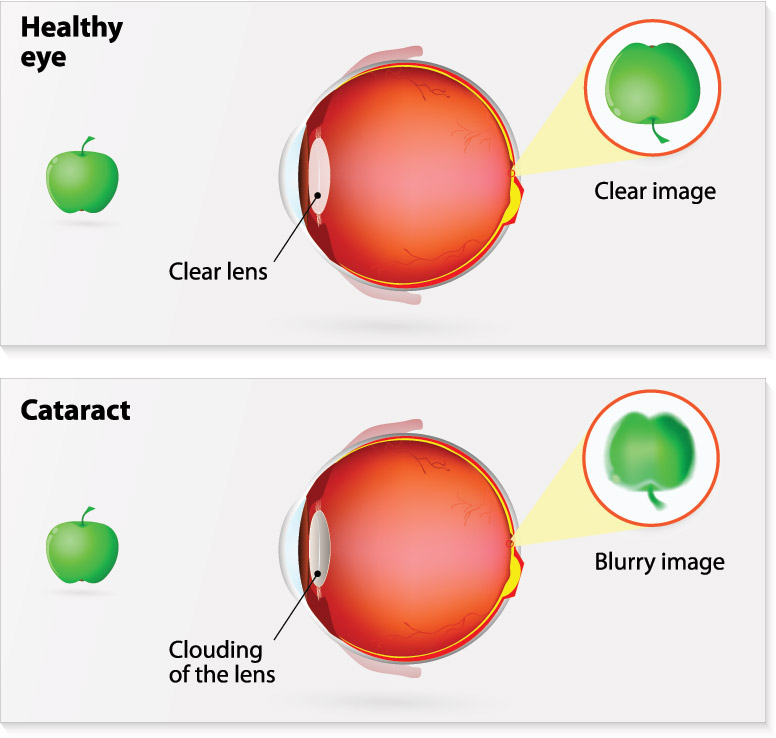
What is cataract?
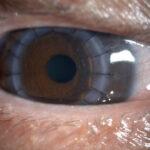
Cataracts are common and occur naturally as we get older. It forms when the lens inside our eye changes with age and becomes less transparent and more cloudy, much like how old glass gets cloudy. Over time, a cataract will progressively get worse, gradually making your vision more blurred.
Who develops cataract?
The main risk factors for developing cataract are as follows:
- Age
- Diabetes
- Trauma (impact to the eye or head)
- Certain medications (such as steroids)
- Eye surgery for other conditions
- Other possible causes: UV exposure,
- smoking & vitamin malnutrition
What are the signs and symptoms?
- Cloudy, fuzzy, foggy or filmy vision
- Alteration in appearance of colours
- Difficulty driving at night
- Severe glare from lights or the sun
- Frequent changes in your spectacle prescription
- Seeing double (even with one eye closed)
- Better near vision for a while
What should I do if I think I have cataract?
Deciding on cataract surgery may not be straight-forward. If you feel your vision is blurred you can get examined by an optometrist or an eye doctor. If new glasses don’t improve your vision and your doctor tells you there are cataracts, then you might want to consider cataract surgery. An eye test can give you an idea of how good your vision is. However, surgery is not recommened simply based on your eye test. You should think about how and whether your quality of life is being affected by your vision. For an example, if you enjoy playing golf or reading, or you need to drive a car, you may want to have cataract surgery sooner.
What if I do not want cataract?
If you choose not to have treatment now, you can always change your mind in the future, if and when your cataracts start to trouble you. It is not advisable to wait until cataracts get very advanced before you opt to have surgery.
Although your sight is likely to be better after you’ve had a cataract removed, you might still need to wear glasses for certain tasks. Therefore, if you can still see well enough with glasses to do the things you want, you may delay having surgery.
Sometimes, people have other eye problems that needs treating, and the cataract is in the way. For an example, some people get damage to the retina because of diabetes etc. If you need surgery for any other condition, your doctor may then recommend that it would be better to have the cataract removed simultaneously. This would also save you having another operation just for the cataract.
Occasionally, another eye condition can mean you won’t get much benefit out of cataract surgery. And if your health is generally poor, surgery may have more risks. If this is the case, it might be better to avoid having an operation. There are things you can do to try to make your life easier. Get new glasses if you need them, as this will maximise your vision. Brighter lighting, especially where you’re reading, will help. Consider getting an angle-poise lamp or similar light-source for your reading area.
When going out in the bright sunlight, anti-glare sunglasses or a hat with a brim can prevent glare from lights and the sun. Lastly, if you still have difficulty, magnifying lenses may make reading easier – just let your doctor know and they can assess you, send you to an optometrist or ‘Low-Vision Aid’ clinic for further evaluation of what tools would suit you best.