A corneal transplant, also known as keratoplasty, is a surgical procedure in which a damaged or diseased cornea is replaced with a healthy cornea from a donor. The cornea is a transparent tissue located at the most front of the eye which helps focus light and contributes to clear vision.
WHO NEEDS A CORNEAL TRANSPLANT?
Several conditions can affect the cornea, leading to vision impairment that cannot be corrected by glasses, contact lenses, or other non-surgical treatments. Some of the common reasons for needing a corneal transplant include:
- Keratoconus: Cornea becomes thinner, steeper and bulges outward into a cone shape.
- Fuchs’ dystrophy: A disease which builds up fluid and results in corneal swelling.
- Corneal scarring (due to injury or infection).
TYPES OF CORNEAL TRANSPLANT
1. Full-thickness (Penetrating Keratoplasty): The entire thickness of the cornea is replaced. This type of transplant is done when the damage affects both the front and inner cornea.

2. Partial-thickness (Lamellar Keratoplasty): Only the front and the middle of the cornea is replaced. This may be done for conditions affecting only the outer layers of the cornea, such as certain corneal dystrophies.

3. Endothelial Keratoplasty: A newer and minimal invasive type of transplant that replaces only the inner layer of the cornea (the endothelium).
THE PROCEDURE
Here’s an overview of how the surgery works:
- Local anesthesia: Before the surgery, eye drops will be instilled to numb the eye.
- Removal of the Damaged Cornea: The surgeon will remove the host’s cornea using a special surgical instrument, leaving a small rim of tissue to hold the donor cornea in place.
- Donor Cornea Placement: Surgeons use fine sutures or air bubbles to attach the donor tissue to the eye. The sutures will be left in place for weeks to months to allow for proper healing.
- Recovery and Follow-up: The healing process can take several months, during which time the patient will need to attend follow-up appointments to ensure the transplant is successful and to monitor for complications.
POSSIBLE COMPLICATIONS
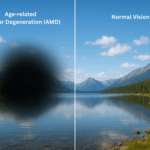
Graft rejection occurs when the body’s immune system sees transplanted tissue as something that shouldn’t be there and tries to get rid of it. This can occur in 3 out of every 10 patients transplanted.
Warning signs of your body trying to reject your cornea transplant include:
- Redness
- Sensitivity to light
- Hazy vision
- Eye pain
Should you experience such symptoms after a transplant, see your corneal surgeon immediately. Your ophthalmologist might be able to stop the rejection with medicine.
CONCLUSION
If you or someone you know is struggling with vision problems due to corneal issues, a consultation with an ophthalmologist can help determine if a corneal transplant might be a viable solution.
The corneal surgeons available in OasisEye Specialists include Dr Vanitha Ratnalingam who is based in Kuala Lumpur and Penang; and Dr K John Mathen who is based in Kuala Lumpur.
FAQs
Donor corneas are sourced from deceased human donors, carefully screened and preserved by certified eye banks. At OasisEye Specialists, donor tissue is mainly obtained from Sri Lanka and the United States, both of which have internationally recognized eye donation systems.
The estimated cost at OasisEye Specialists is approximately RM15,000 to RM20,000 per eye. Costs may vary based on individual clinical needs.
Typically, the procedure takes about 1 to 2 hours, depending on the type of transplant.
Recovery varies but often takes several months to a year for full vision stabilization. Regular follow-ups are essential.
Vision usually improves gradually over weeks to months after surgery. Sometimes, additional procedures like glasses, contact lenses, or refractive surgery may be needed for best results.
Usually, surgery is done on one eye at a time to reduce risk.
With proper care, many grafts last 10 to 20 years or more, though some may fail earlier.