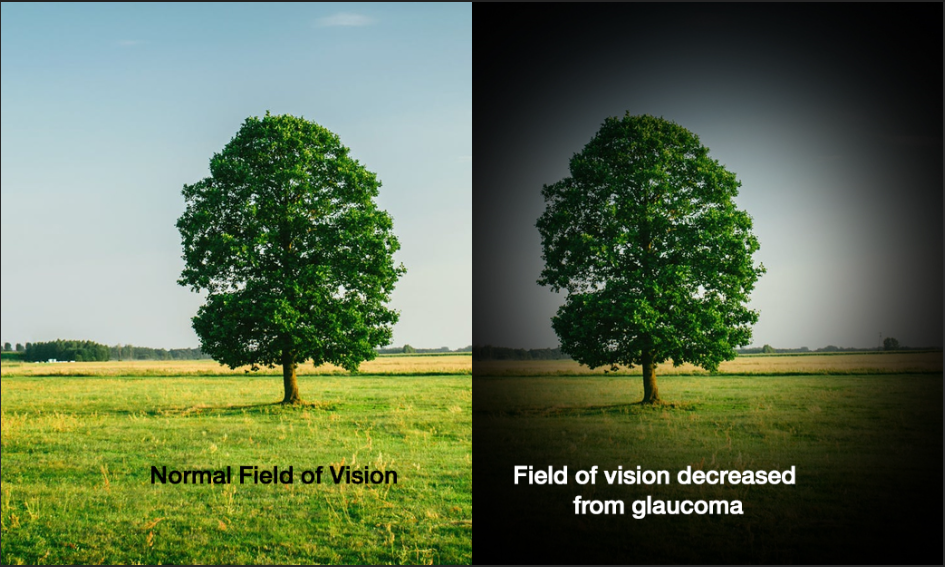
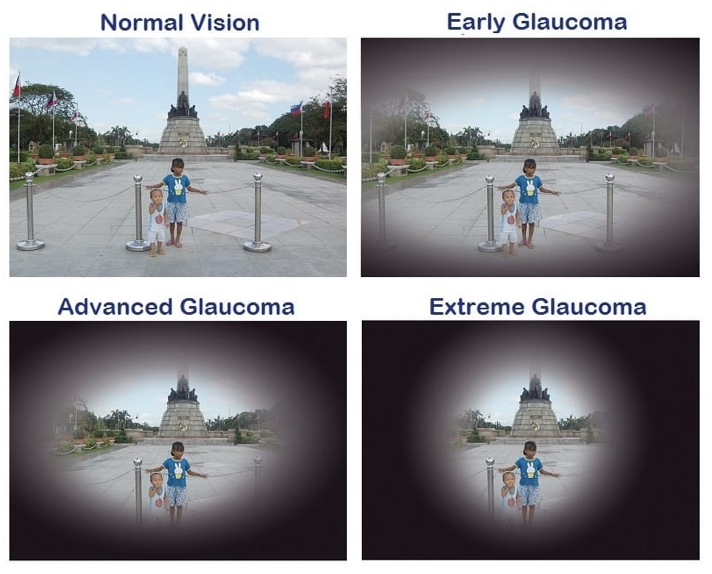
Glaucoma is a progressive disease that affects the optic nerve of the eye. The optic nerve is part of the central nervous system (CNS) and is the ‘cable’ that connects the eye to the brain. Once it is damaged, it cannot regenerate (repair itself). As nerve fibers of the optic nerve die slowly due to glaucoma, peripheral vision is also lost gradually. People with advanced glaucoma may experience “tunnel vision”, in which they can only see objects in the center of their visual field. The image below is an illustration of vision of a person with glaucoma.
 What makes glaucoma more dangerous is that the most common type of glaucoma does not show any obvious symptoms, hence goes undetected in many people. Thus, glaucoma is known as the “silent thief of sight”.
What makes glaucoma more dangerous is that the most common type of glaucoma does not show any obvious symptoms, hence goes undetected in many people. Thus, glaucoma is known as the “silent thief of sight”.
Glaucoma is one of the leading causes of irreversible blindness and therefore it is important to know the risk factors that can lead to this disease.
Strong risk factors for Glaucoma are:
- Advancing age (over 60 years old)
- Certain races are more predisposed than others (Blacks/ Hispanics/ Asians )
- Family history (1st degree relatives)
- High baseline Intraocular pressure (IOP)
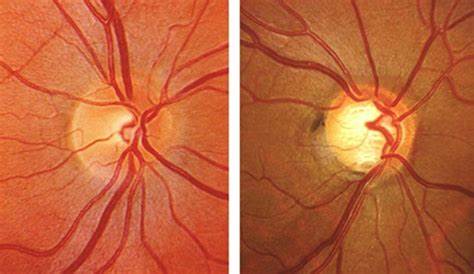
- Suspicious optic nerve appearance / asymmetry
Possible risk factors are:
- Myopia (Near sightedness)
- Vascular disorders – Diabetes/ Hypertension/ hypercholesterolemia)
- Previous eye injury/ eye surgery
Other risk factors are:
- Long term use of steroids (eye drops/ creams/ oral/ inhalers/any other form)
- Migraine headaches (vasospasms)
- Sleep related breathing disorder (sleep apnea)
- Hypotension (low blood pressure)
One should have regular eye examinations as early detection is key to preventing further vision loss from glaucoma. According to guidelines by American Association of Ophthalmology (AAO), adults who have no signs or risk factors for eye disease should have a comprehensive eye examination at age 40 if they have not received one. For asymptomatic individuals without risk factors who are 40 to 54 years old, and have had a comprehensive eye examination, the recommended interval is once every 2-4 years. For those aged between 55 and 64, they should get an eye examination every 1-3 years. Anyone aged 65 or older should have an eye examination every 1-2 years, despite not having any symptoms.

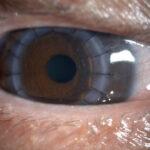
By consulting a glaucoma specialist, the doctor is able to examine your eyes and determine if you have glaucoma. With the help of equipment such as the applanation tonometer, optical coherence tomography (OCT), visual field analyser, and fundus camera, the doctor is able to detect subtle changes in your optic nerve and retina.
Screening of higher-risk groups may be the most cost-effective method of reducing the volume of undiagnosed glaucoma and patient history appears to be a practical means of screening to identify the higher risk individuals.
There is a risk that if glaucoma is not detected early, irreversible loss of vision may occur, and that would affect the quality of life. Residents within Klang Valley in areas such as Cheras, Puchong, Shah Alam, and Kepong can come visit our glaucoma specialist, Datin Dr Thayanithi to have their eyes examined.