Hydroxychloroquine is a controlled medication for several dermatologic and rheumatologic conditions. It is also widely used to treat Systemic Lupus Erythematosus (SLE) disease and Malaria (by using Chloroquine originally). The maximum recommended dose is 5 mg/kg/day, which is commonly used in SLE patients. Recent research trials suggested that high-dose HCQ is a potential use for coronavirus, COVID-19 therapy by reducing viral replication, but there is insufficient evidence supporting its efficacy. Ongoing long-term usage and high doses of hydroxychloroquine can cause unwanted side effects to the body, including the eyes.
Side effects
- Dizziness
- Headache
- Ocular toxicity
- Skin rash
- Gastrointestinal upset such as diarrhoea, vomiting and stomach cramps
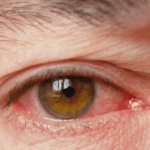
In severe cases, seizures, angioedema, arrhythmia, and bronchospasm may occur. Long-term hydroxychloroquine usage can cause toxicity to the eyes as well, including the cornea, ciliary body and retina.
Eye diseases
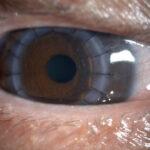
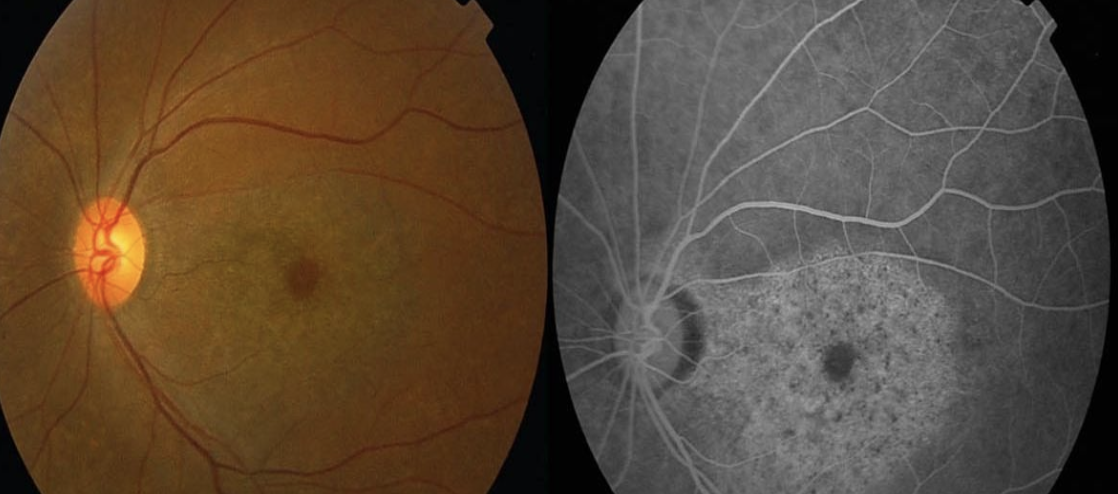
Chloroquine was initially used to help treat malaria. Chloroquine is less often used now because its derivative hydroxychloroquine is better. Hydroxychloroquine is commonly used to treat inflammation in diseases like rheumatoid arthritis and dermatitis. The toxic effects of this substance on the retina are seen in the area known as the macula. Some people may have early signs of toxicity, such as changes in their vision. More advanced toxicity may involve complaints like difficulty seeing in colour or a scotoma (a dark spot in the centre of your vision). Advanced hydroxychloroquine toxicity can cause a bull’s eye maculopathy. Since retinal toxicity is usually irreversible, finding out if someone has retinal toxicity and stopping the thing that is causing the toxicity as soon as possible is the best treatment. Corneal toxicity is when a drug gets deposited into the cornea. This is very rare, and it typically doesn’t affect vision. In rare cases, ciliary body dysfunction can happen and influence the eye from focusing.
Risk factors
Hydroxychloroquine retinopathy is more common in patients with longer duration and daily dosage of the drug. Patients are at higher risk of retinopathy if they use hydroxychloroquine for more than 5 years as treatment.
 Signs
Signs
Hydroxychloroquine retinopathy is usually bilateral and symmetric. The early signs include macular edema and granular depigmentation in the retinal pigment epithelium in the retina. It can progress to an atrophic bull’s eye maculopathy if continuous drug exposure causes widespread other areas of the retina, including the optic nerve. Hydroxychloroquine keratopathy is seen as an intraepithelial deposit. Ciliary body dysfunction can be detected when the near vision is poor.
Symptoms
Initially, hydroxychloroquine toxicity may cause few or no symptoms. However, over time, symptoms may develop such as hard to differentiate colour, loss of central vision, reading difficulty, blur of vision, glare, flashing of lights, and metamorphopsia. It usually affects both eyes. In keratopathy, patients may experience halos around light and photophobia whereas in ciliary body dysfunction, will complain of reading difficulty and find it hard to focus on near work.
Treatment
Early detection of hydroxychloroquine toxicity can be stopped to prevent further retinal damage and visual loss. Patients who start hydroxychloroquine as medical condition treatment should be on regular eye examination, especially those who are exposed to drugs for more than 5 years. There is no treatment that can be done by surgery at the moment. Hydroxychloroquine retinopathy is not reversible, as the damage appears to continue for a period of time. However, the early detection of retinopathy can prevent further visual deterioration. It can be treated in keratopathy cases. If you are a patient with ongoing hydroxychloroquine, it is advisable to have an eye examination with an ophthalmologist to rule out any eye disease.