What are floaters?
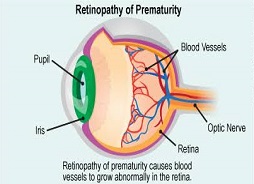
Have you ever noticed little tiny black dots in your vision? These are usually called floaters in layman’s terms. Floaters are usually more noticeable in a bright environment or a bright blue sky on a sunny day. Floaters can come in different shapes such as little dots, circles, lines, clouds or cobwebs. It may be of a sudden onset and it is usually due to the vitreous which is the jelly inside your eye shrinking due to age. This process occurs especially when you’re growing older or if you’re very short sighted (myopia) then you would get it earlier. However, it can come about in other conditions as well such as in diabetes and when you have an infection or inflammation in your eye. In most people this is an innocuous or relatively minor problem that happens as you get older.
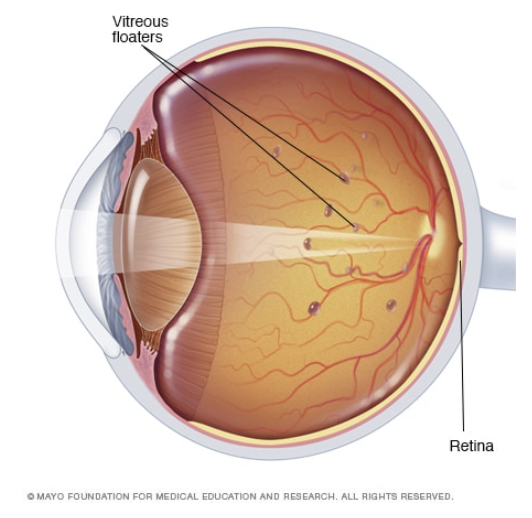
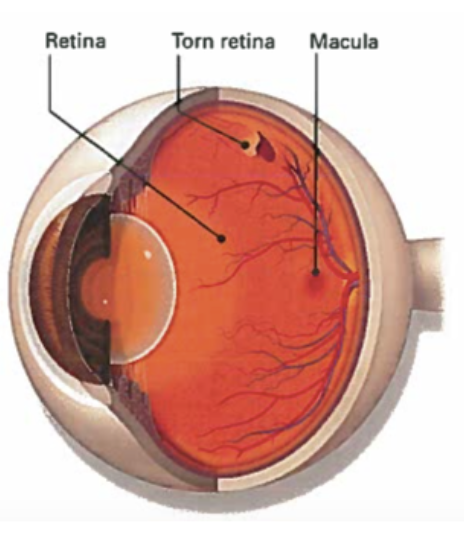
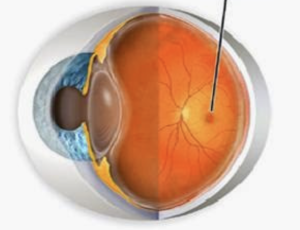
Floaters are normal and a common part of aging. However, at least 1 percent of the time, the shrinking of the vitreous or the jelly may happen. It starts from peeling off your retina. The retina is a thin layer inside your eye that is full of nerve tissues which is like the film in a camera and is what you use to see things. Now if this jelly shrinks and pulls on your retina too hard, it can sometimes cause a tear. If there is a tear, you will need treatment for it. The incidence of this is about 1 percent so most of the time nothing needs to be done. However, we also need to rule out other problems such as infection or inflammation or perhaps bleeding in the eye. While floaters are typically harmless, if it appears suddenly and accompanied with flashes of light or impaired vision, it can signal a potential serious eye problem.
What are flashes of light?
Flashes look like flashing lights or lightning streaks in your field of vision. Flashes happen when the vitreous pulls on the retina. In younger people, the gel inside the eye (vitreous) is firmly attached to the retina. As you get older, the vitreous gel becomes more liquid and slowly collapses away from the retina. Flashes can be a symptom of a retinal tear or retinal detachment. A retinal tear is a break in the retina while a retinal detachment is when the vitreous pulls away, creating a break and fluid from the vitreous gets behind the retina causing blurred vision. These are serious conditions that can damage your sight. Flashes are usually seen in people as they age or those with migraines. Flashes can appear on and off for several weeks or months. Flashes that are caused by migraine usually happen among the younger people. When you have a migraine it causes flashes that look like jagged lines or heat waves. This can occur in one or both eyes and can last up to 20 minutes.
Treatment
Treatment of floaters and flashes depends on the underlying condition. A thorough eye examination by an Ophthalmologist will determine if there are any damages to the retina. While some floaters will remain in your vision, many of them will fade over time and cause less problems. However, for large floaters that obstruct daily tasks, a vitrectomy surgery can be performed to remove the vitreous gel inside the eye and will be replaced with a bubble of air or gas. The gas will disappear over time and will be replaced with a clear fluid produced by the eye.

What can you do about floaters and flashes in your eye?
It is important to take care of your eyes as you age. If you notice occasional eye floaters or flashes in your vision is not something you should worry about. This is normal and often happens when you age. An increased number of floaters in your vision or flashes should be a call for an emergency. When this occurs, it is wise to see an Ophthalmologist immediately to avoid any vision loss. Make an appointment to see an Ophthalmologist if you experience any of the warning signs below:
- A new onset or increase in floaters or flashes of light
- A sudden increase in size and number of floaters
- A sudden change or decline in vision








 Makula adalah satu kawasan kecil di bahagian tengah retina yang memiliki banyak sel penglihatan. Punca utama degenerasi makula kering masih tidak dapat dikenalpasti. Tetapi penyelidikan menunjukkan ianya mungkin dipengaruhi oleh faktor genetik dan factor persekitaran, termasuk merokok, obesiti dan diet. Apabila umur semakin meningkat, bermula pada usia 55 tahun dan keatas sesetengah berlakunya perubahan negatif pada makula. Kekurangan zat juga menyebabkan sel-sel di makula rosak dan tidak dapat berfungsi dengan baik. Perubahan ini menyebabkan penglihatan menjadi kabur sehingga menjadi buta.
Makula adalah satu kawasan kecil di bahagian tengah retina yang memiliki banyak sel penglihatan. Punca utama degenerasi makula kering masih tidak dapat dikenalpasti. Tetapi penyelidikan menunjukkan ianya mungkin dipengaruhi oleh faktor genetik dan factor persekitaran, termasuk merokok, obesiti dan diet. Apabila umur semakin meningkat, bermula pada usia 55 tahun dan keatas sesetengah berlakunya perubahan negatif pada makula. Kekurangan zat juga menyebabkan sel-sel di makula rosak dan tidak dapat berfungsi dengan baik. Perubahan ini menyebabkan penglihatan menjadi kabur sehingga menjadi buta.