Uveitis is the inflammation of the uvea (the middle layer of the eye), which includes the iris, ciliary body, and choroid. It can cause eye pain, redness, blurred vision, light sensitivity and floaters.
Types of Uveitis
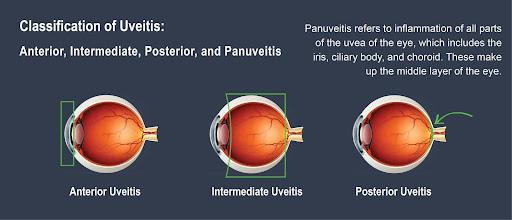
Source: Tennessee Retina
Causes of Uveitis
Uveitis can have various causes, which are often classified into the following categories:
1. Autoimmune and Inflammatory Conditions
- Ankylosing spondylitis
- Rheumatoid arthritis
- Juvenile idiopathic arthritis
- Sarcoidosis
2. Infections
- Bacterial, viral, fungal, or parasitic
3. Trauma or Injury
- Direct eye trauma or injury
- Secondary to eye surgery
4. Other Cause or Risk Factors
- Smoking
- Cancer related
- Genetics: certain genetic markers, such as HLA-B27
- Idiopathic (no identifiable cause)
Symptoms of Uveitis
Symptoms can develop suddenly or gradually and may affect one or both eyes. Common symptoms include:
- Eye pain (aching or throbbing)
- Redness in the eye
- Blurred vision
- Sensitivity to light (photophobia)
- Floaters (small dark spots in vision)
Diagnosis of Uveitis
- Dilated Eye Examination: The doctor will use eye drops to widen your pupils, allowing them to check the structures in the back of your eye.
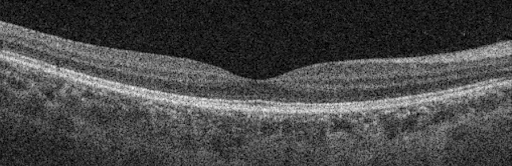
- Optical Coherence Tomography (OCT): This imaging technique provides detailed cross-sectional images of the retina, showing the separation of retina layers.

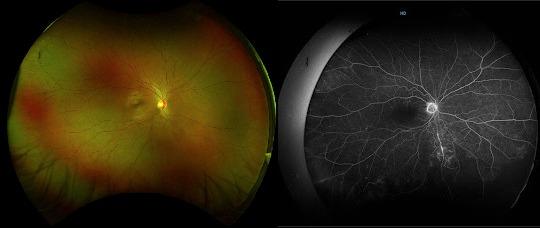
- Widefield Retinal Imaging: It provides a field of view of 200 degrees or 82% of the retina in a single capture. Besides, using special dyes injected into the bloodstream, Fundus Fluorescein Angiography (FFA) or Indocyanine Green Angiography (ICGA) can help to detect blood vessel leakage or fall out which might be caused by uveitis.

- Laboratory Investigations: Several examinations including blood test, ESR, PCR test or Chest X-ray could rule out the underlying autoimmune or infectious causes.
Treatments of Uveitis
The treatment of uveitis depends on the underlying cause, severity, and part of the eye affected (anterior, intermediate, posterior, or panuveitis). Here’s an overview of common treatments:
1. Medications
A. Corticosteroids (to reduce inflammation)
B. Immunosuppressive or Biologic Therapy (for non-infectious or autoimmune uveitis)
C. Antimicrobials (if infection is the cause)
D. Cycloplegic Drops (to relieve pain and prevent complications)
2. Lifestyle and Supportive Measures
- Sunglasses – to reduce light sensitivity
- Regular eye exams – to monitor progress
- Managing underlying conditions – such as autoimmune diseases
3. Surgery (for severe or refractory cases)
- Vitrectomy – to remove inflammatory debris or treat complications
- Cataract or glaucoma surgery – if secondary complications develop
Why Early Diagnosis Matters
If left untreated, uveitis can lead to complications such as glaucoma, cataracts, macular edema, or even permanent vision loss. Early diagnosis and prompt treatment are key to preventing serious outcomes.
If you experience persistent eye pain, redness, or changes in your vision, don’t wait—consult an eye care professional.
The medical retina & uveitis specialists available in OasisEye Specialists include Dr Wong Hon Seng who is based in Kuala Lumpur; Dr Rajasudha Sawri Rajan who is based in Kuala Lumpur and Puchong.
FAQs
Yes. If not treated properly, uveitis can lead to complications such as:
- Glaucoma
- Cataracts
- Retinal damage or detachment
- Vision loss or blindness
Early diagnosis and treatment are critical.
Treatment depends on the cause, severity, and type. Options include:
- Steroid eye drops (mainstay for anterior uveitis)
- Oral steroids or injectable steroids
- Immunosuppressive medications (for autoimmune-related cases)
- Antibiotics or antivirals (for infectious causes)
- Mydriatic drops (to dilate the pupil and reduce pain)
Treatment aims to control inflammation, prevent complications, and preserve vision.
Yes, recurrence is common, especially in autoimmune-related uveitis. Long-term monitoring is important even after symptoms resolve.
Most forms of uveitis are not contagious, but if caused by an infection like herpes or tuberculosis, the underlying infection might be.
- Treat underlying conditions properly (autoimmune diseases, infections)
- Protect your eyes from injury
- Attend regular eye exams if you have a history of uveitis or autoimmune disease
- Follow your doctor’s treatment plan to prevent recurrences
See an eye doctor (ophthalmologist) immediately. Early treatment can prevent serious complications.