Alcohol, a psychoactive substance with dependence-producing properties, has been widely used in many cultures for centuries, according to the World Health Organization (WHO). Although alcohol consumption is often associated with people having a good time and enjoying themselves, taking it too far can have serious consequences on your health.
Most people associate heavy drinking with liver disease or accidents, but did you know that alcohol can also have an impact on your eyes? Excessive alcohol consumption can cause both short and long-term effects on your vision and eye health, and it’s important to be aware of both.
Short-term effects of alcohol on your vision
Short-term effects of alcohol on your vision can impair your peripheral vision and lead to tunnel vision. Alcohol hinders your pupils’ ability to react, preventing them from constricting or dilating properly. Car headlights, for example, can directly slow your reaction time, making it challenging to do simple tasks like driving at night. This is one of the key reasons why it is risky and against the law to drive after drinking.
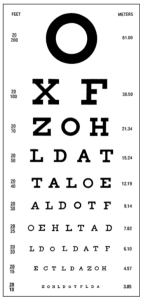
Furthermore, alcohol can cause blurry and distorted vision, which everyone reacts to differently depending on the amount consumed. There is a delay between the brain and the eyes due to the slow rate of communication between neurotransmitters in the brain, which weakens eye muscle coordination. Alcohol can also affect one’s capacity to perceive contrast, reducing it by 30% at the permissible blood alcohol level, according to a study. Contrast is the visual system’s processing of differences in brightness and is the root cause of this temporary impairment, making it more difficult to distinguish between different objects based on lightness and darkness, such as traffic lights.
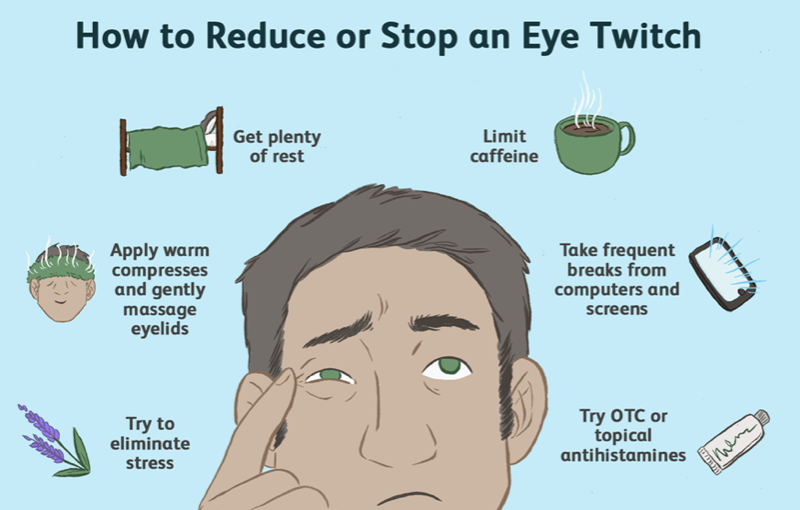
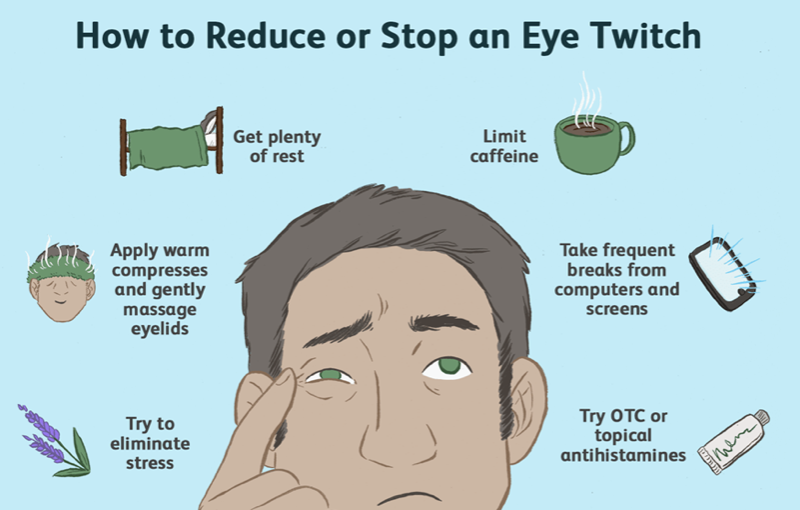
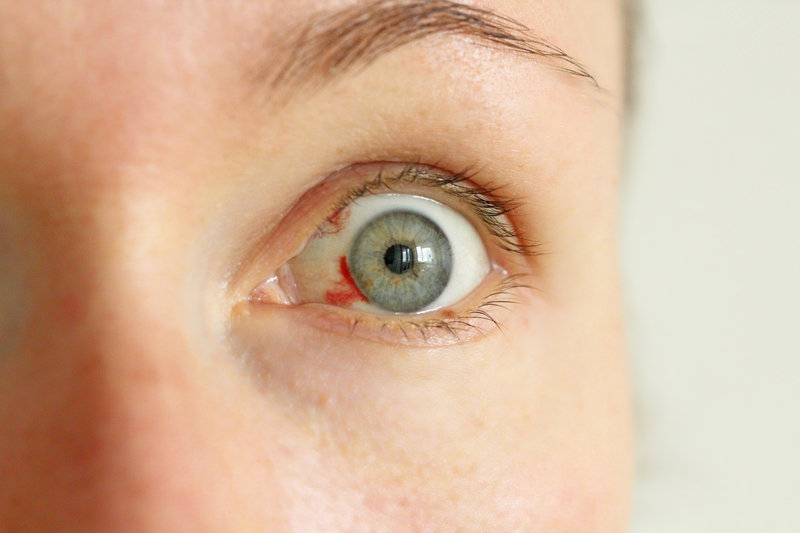
Excessive or regular alcohol intake can also cause dry eyes and myokymia, or twitching of the eyelids, resulting in temporary inflammation, double vision, eye burning and itching, migraines, and sensitivity to light. The long-term consequences of these symptoms include expanded blood vessels in the eyes, making them often appear red and bloodshot.
Long-term effects of alcohol on your vision
Regular alcohol consumption over time can also increase the risk of early cataract formation, which can start to manifest as early as age 40. Long-term impairments may also include permanent blurring of vision or double vision caused by the weakening of the eye muscles, resulting in a slower reaction time.
Moreover, prolonged alcohol abuse can affect your vision due to vitamin deficiencies. Heavy drinking can interfere with the liver’s ability to absorb vitamins essential for maintaining healthy eyes and good vision. Alcohol can only be broken down by the liver so quickly.

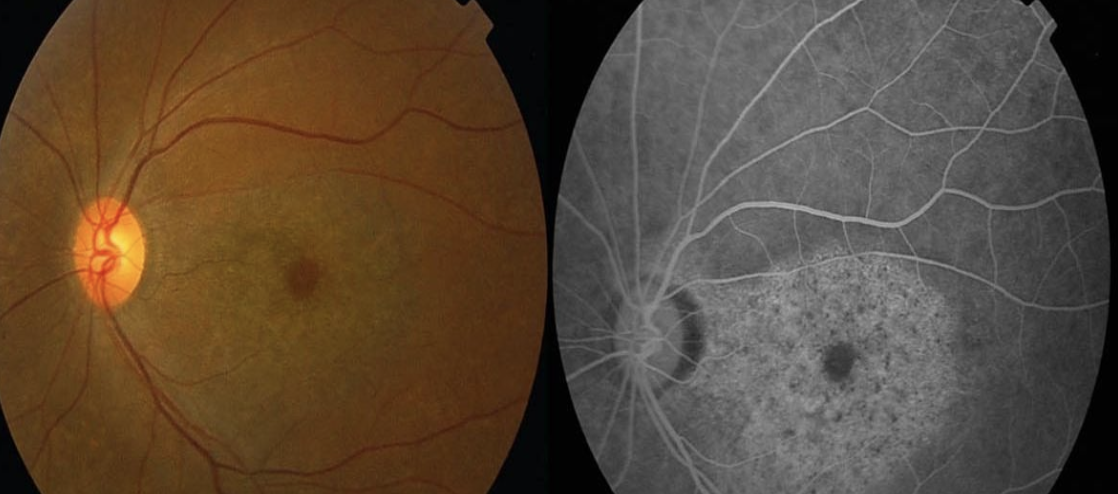
Drinking too much alcohol may make you more susceptible to age-related macular degeneration (AMD). According to WHO research, the average person consumes 33g of pure alcohol every day, which is equivalent to two glasses of wine. Based on an Australian study, people who drink more than 20g of alcohol per day have a 20% higher risk of developing early AMD than those who don’t drink at all.
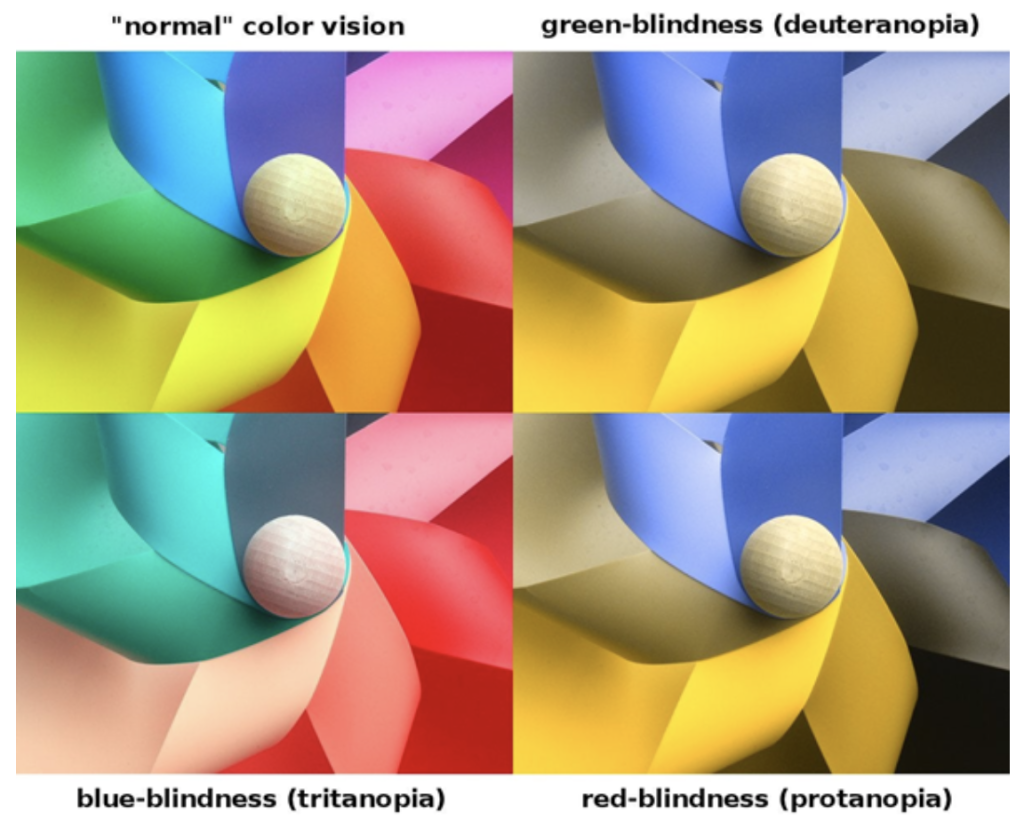
Optic neuropathy or optic atrophy is one of the most dangerous effects of long-term alcohol use on vision. This disorder, brought on by excessive drinking or smoking, is also known as tobacco-alcohol amblyopia or toxic amblyopia. It causes a painless loss of eyesight, as well as diminished colour vision and peripheral vision. Alcohol increases the risk of heart disease, and heart disease symptoms can be seen in the eyes, including optic neuropathy, atrophy, bleeding in the retina from vascular occlusions, and even hypertensive retinopathy.










 Signs
Signs