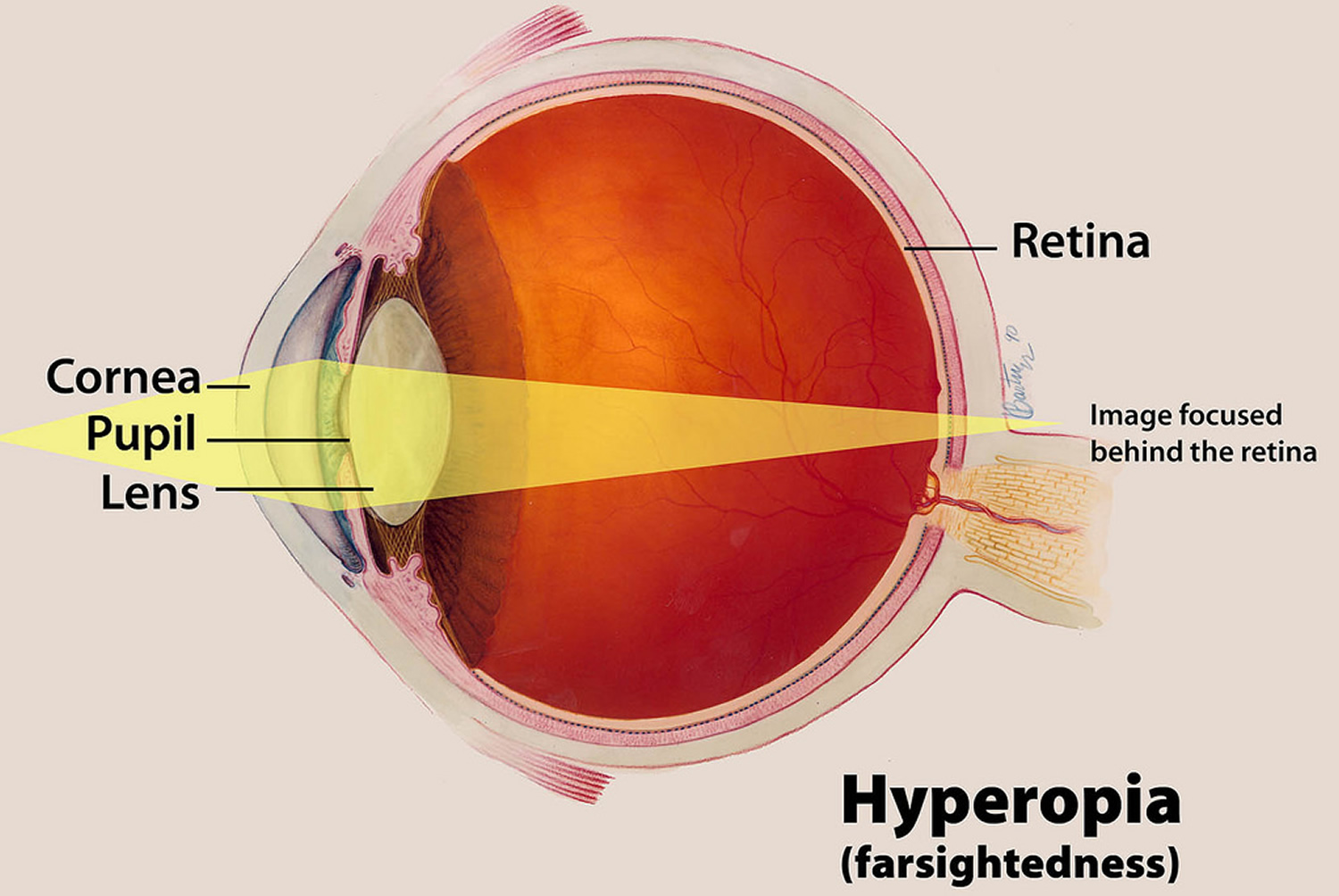
Astigmatism (散光 in Mandarin / ‘silau’ in Malay) is a common type of refractive error that can cause blurred or distorted vision. Other types of refractive errors are myopia (short-sightedness), hyperopia (long-sightedness) and presbyopia. Astigmatism is usually caused by an imperfection in the curvature of the cornea, causing a person to see images that are blur or not in focus at all distances.
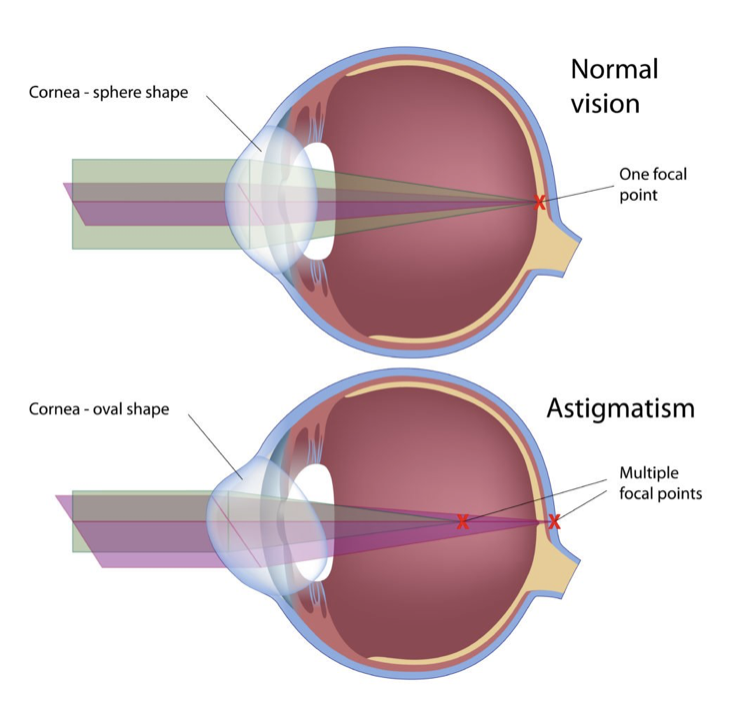
If your cornea is almost perfectly round in shape, it is able to focus light onto a single point. However if both your cornea and lens is more oval than round, instead of focusing onto a single point, it focuses on multiple points on the retina (back of the eye). When the cornea or lens shape is highly irregular, a person may experience significant blur vision at all distances.
Who is at risk for astigmatism?
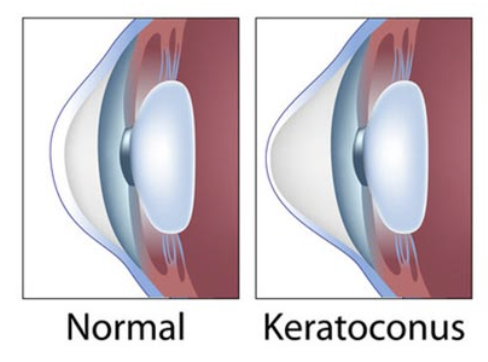
Astigmatism can affect both children and adults. It may be congenital, or present at birth due to the natural shape of the eye. In babies, astigmatism usually resolves by the first year of life. However, there are some children who do not outgrow astigmatism and this can negatively impact their learning and development. Thus, it is necessary to schedule for periodic eye examinations for children to detect astigmatism or other refractive errors. Parents who have been diagnosed with high astigmatism should get their child’s eye tested for severe astigmatism as it is believed to be hereditary. Some people can also develop astigmatism after an eye injury or surgery. Those with a family history of keratoconus (degeneration of cornea) should also get their eye tested for high astigmatism at an early age.
What are the symptoms of astigmatism?
The most common symptom of astigmatism is blurred and distorted vision at all distances. Many people with low astigmatism may not have any symptoms. Those with astigmatism of 0.75D and above will start to have noticeable symptoms. These signs and symptoms include headache, eye strain and squinting to see clearly. Astigmatism can also cause shadowing of images which makes letters appear double. Night vision can also be poor due to debilitating glare and halos around lights.

What are the treatment options for astigmatism?
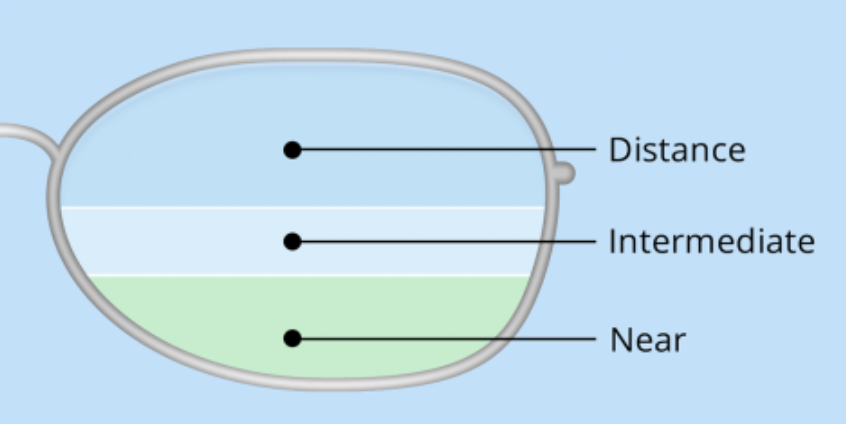
If the astigmatism is mild, your eye care practitioner may suggest no treatment at all. If you have moderate to high astigmatism, corrective lenses, either glasses or contact lenses are the most suitable treatment options. Eyeglasses contain a special cylindrical lens prescription to correct astigmatism. Both soft toric contact lenses and rigid contact lenses can correct astigmatism. For high astigmatism (above 3.00D), rigid gas permeable lenses may be a better option. Surgical treatments of astigmatism include refractive surgery by reshaping the cornea via TransPRK or implantation of ICL. If you have cataract in your eyes, a toric IOL can be implanted in your eye to simultaneously remove the cataract and correct astigmatism.
How is astigmatism diagnosed?
A comprehensive eye examination by an optometrist or ophthalmologist will help to diagnose astigmatism. Children who have astigmatism rarely report it to their parents. Therefore, parents should look out for signs and symptoms in their children such as eye rubbing, squinting to see things, moving closer to see things and closing of one eye. Regular eye examinations are important to maintain a high quality of life and productivity.















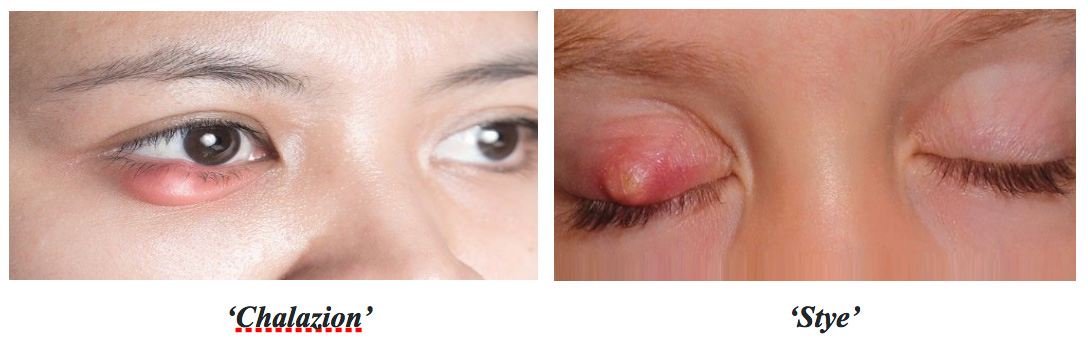 Bagaimanakah cara untuk anda menyembuhkan ketumbit?
Bagaimanakah cara untuk anda menyembuhkan ketumbit?


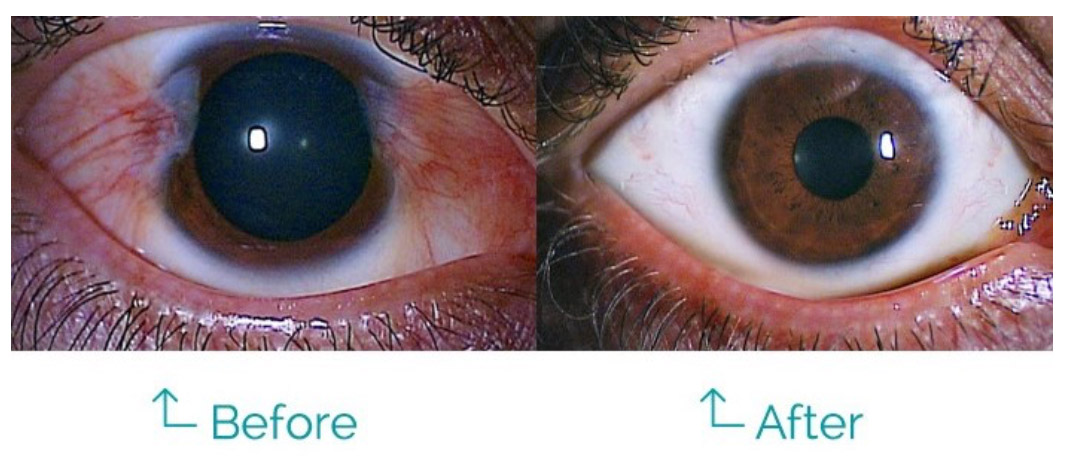


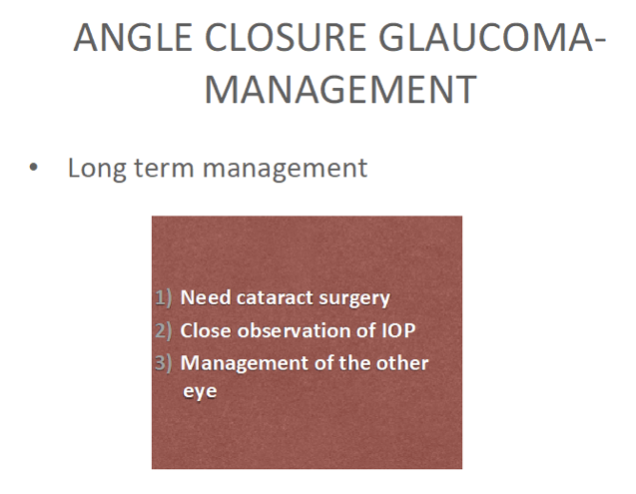
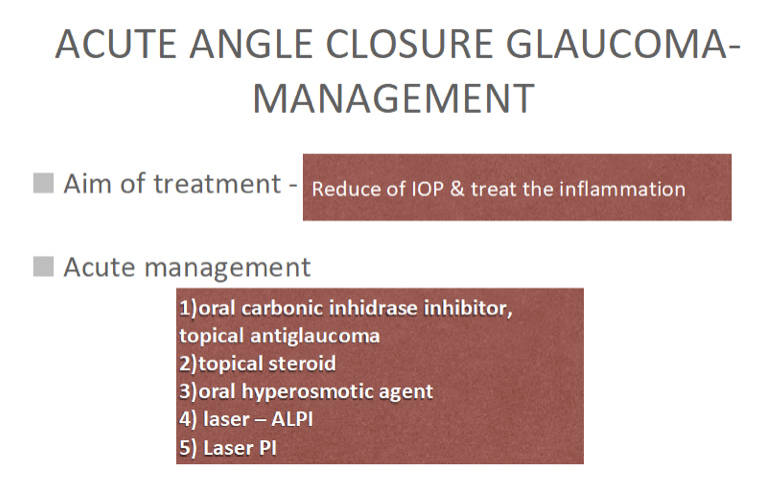 Once the IOP is controlled with laser treatment and anti-glaucoma medications and the affected eye has stabilized, there is a need to plan for cataract surgery in the future. All these are done to reduce and prevent irreversible damage to the optic nerve and thus maintain quality of life.
Once the IOP is controlled with laser treatment and anti-glaucoma medications and the affected eye has stabilized, there is a need to plan for cataract surgery in the future. All these are done to reduce and prevent irreversible damage to the optic nerve and thus maintain quality of life.