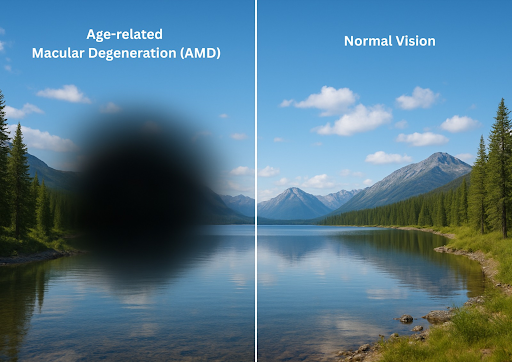
Age-related macular degeneration (AMD) is a chronic and painless disease of the macula that can blur your central vision. The macula is part of the retina, which is the light-sensitive tissue at the back of the eye that mainly controls sharp, detailed vision. AMD is a common condition that causes visual loss in those over 50. As we age, the macula can undergo damage, thinning, or abnormal blood vessel growth, leading to vision loss.
Types
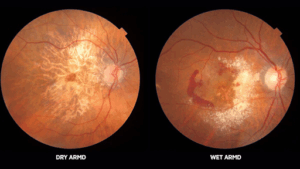
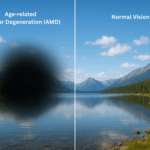
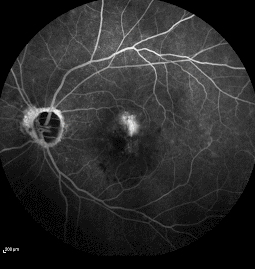
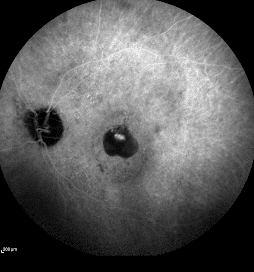
Source: NEORETINA Eyecare Institute
There are 2 types of AMD: dry and wet.
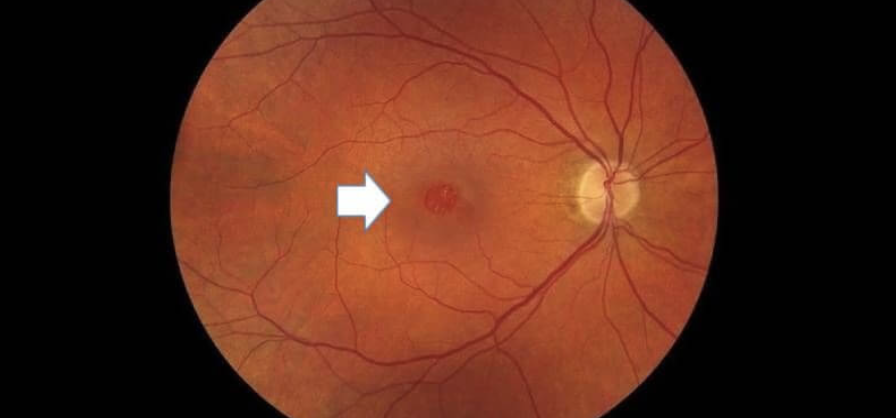
Dry AMD, also known as atrophic AMD, affects the majority of AMD patients. It occurs when the light-sensitive cells in the macula slowly break down, gradually blurring central vision in the affected eye.
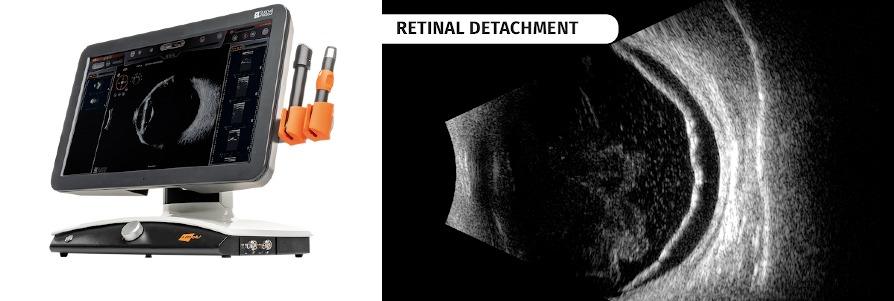
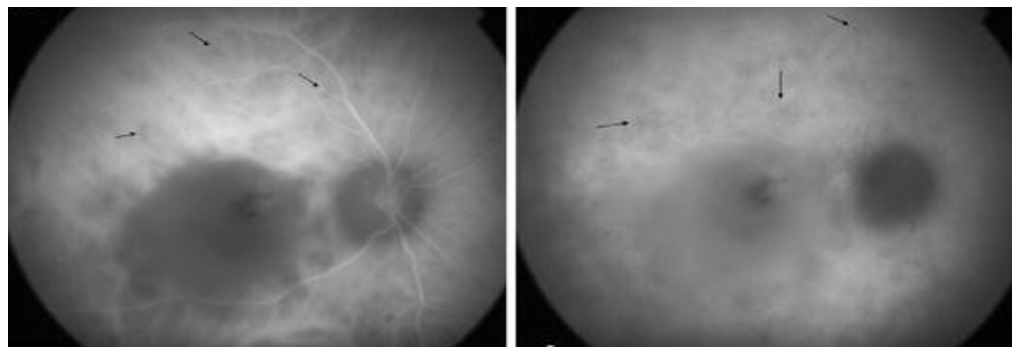
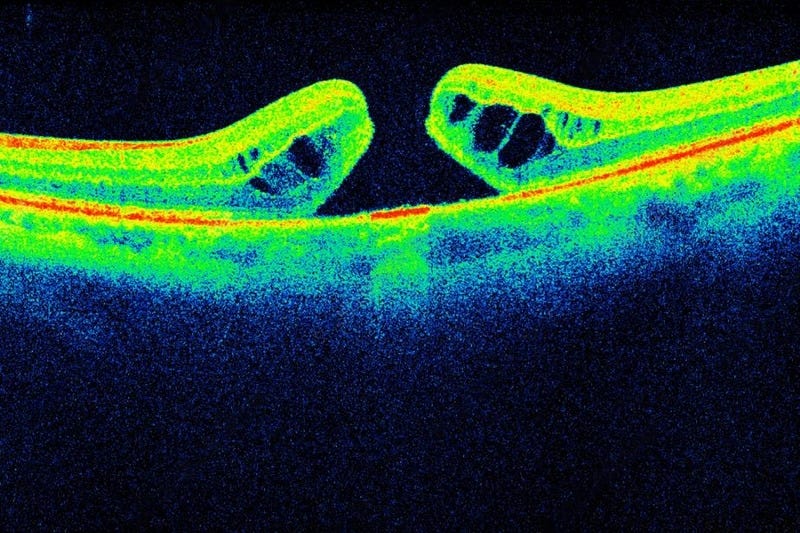
A less common kind of AMD that typically results in rapid vision loss is wet AMD, also known as neovascular AMD. It occurs when abnormal blood vessels grow in the back of the eye.
Symptoms
- Difficulty seeing in dim light
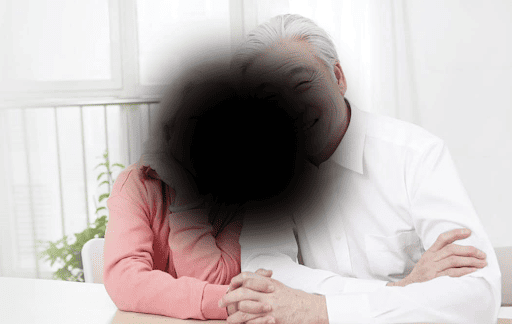
- Blurriness in their central vision
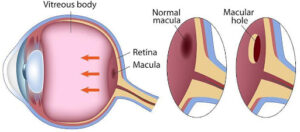
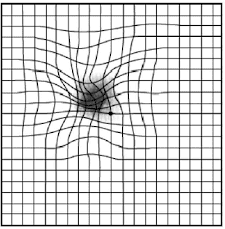
- Straight lines begin to appear crooked or wavy
- Hazy patch (blind spot) close to your centre vision
- Colors appear less bright/saturated
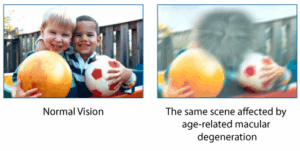
Source: National Eye Institute, National Institutes of Health
Straight lines looking wavy are a warning sign for late AMD. If you notice this symptom, see your eye doctor right away.
Risk factors
People aged 55 and older are more likely to have AMD. The risk for AMD is also higher for those who:
- Have a family history of AMD
- Caucasian
- Women
- Smoking
- Lack of physical activity
- High blood pressure (hypertension) and high cholesterol levels
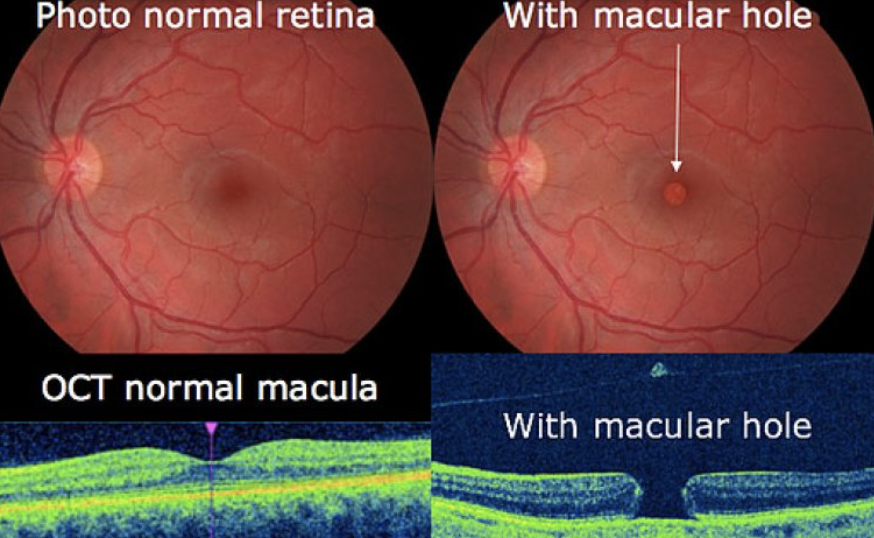
Assessment
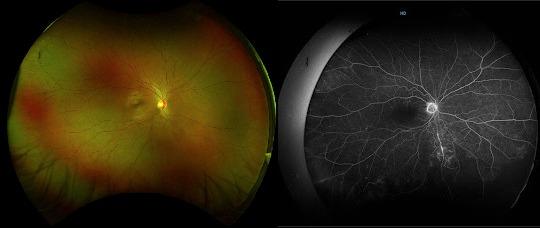
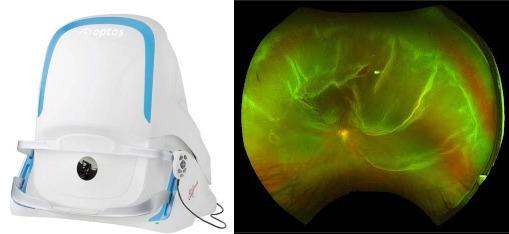
- Dilated eye examination.
- Amsler chart. This can detect hazy, wavy or missing lines or areas on the grid.

Source: Pujashah
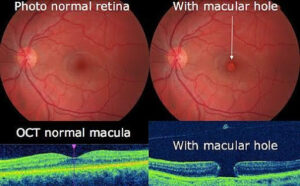
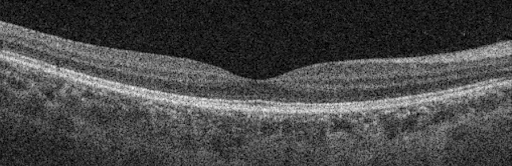
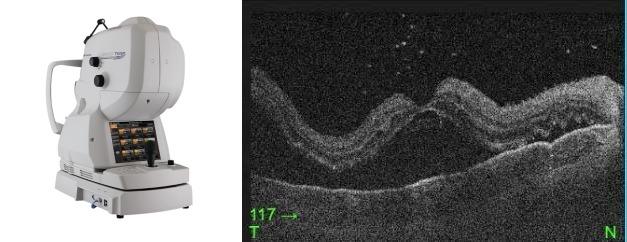
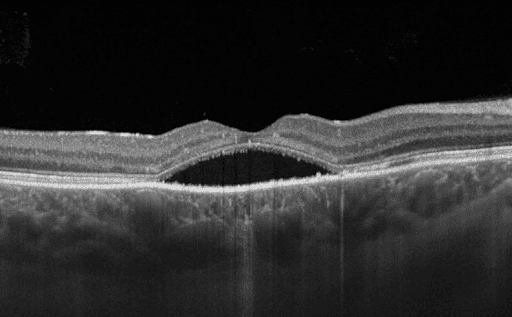
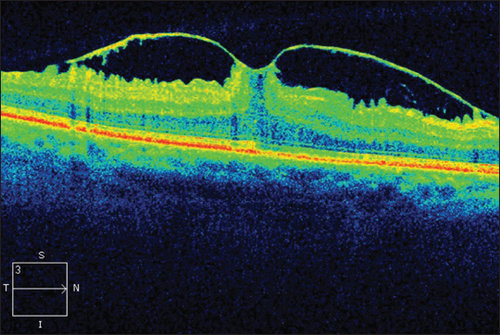
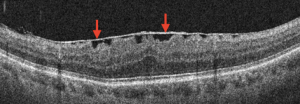
- OCT scan. A non-invasive and painless scan for your retina and macula.

Treatment
Since there is currently no cure for early AMD, your eye doctor will most likely use routine eye exams to monitor the condition of your eyes. Healthy eating, frequent exercise, and quitting smoking can all be beneficial as well.
Certain dietary supplements, such as vitamins and minerals, may be able to prevent AMD from progressing to the late stage.
On the other hand, if you have wet AMD, there are other treatments that may be able to stop further vision loss:
- Anti-VEGF injections are the standard treatment involving injections in your eye used to slow the progression of the disease and reduce the damaging effects of these leaky abnormal blood vessels.
- Photodynamic therapy (PDT), a combination of injections and laser treatment. A light-sensitive drug is injected into the bloodstream, where it concentrates in abnormal blood vessels below the macula. The drug is then activated by a laser beam that is directed into the eye, resulting in the formation of blood clots, which seal off the abnormal blood vessels.
- Laser photocoagulation is used to delay the progression of vision loss by sealing off abnormal blood vessels with a laser.
Currently, there is no effective treatment to reverse vision loss in late-stage dry AMD, but support is available to help you live with AMD, including help with low vision and lifestyle changes in order to help you have the best quality of life.
The retinal specialists available in OasisEye Specialists include:
- Dr Kenneth Fong Choong Sian – Kuala Lumpur
- Dr Manoharan Shunmugam – Kuala Lumpur
- Dr Wilson Wong Jun Jie – Kuala Lumpur
- Dr Wong Hon Seng – Kuala Lumpur
- Dr Rajasudha Sawri Rajan – Kuala Lumpur, Puchong
- Dr Ling Kiet Phang – Johor Bahru
- Dr Teh Wee Min – Seremban
- Dato Dr Haslina Binti Mohd Ali (D.S.D.K) – Penang
FAQs
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Ut elit tellus, luctus nec ullamcorper mattis, pulvinar dapibus leo.
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Ut elit tellus, luctus nec ullamcorper mattis, pulvinar dapibus leo.